Vasectomy Reversal:Vasovasostomy and Epididymovasostomy Details
Vasectomy reversal is receiving increasing attention in urologic practice. The most common situation involves the remarriage of a man who has previously had a vasectomy and now desires additional children. Vasectomy reversals are also requested by couples who have long-standing marriages but simply have decided to have additional children. Fortunately, microsurgery has advanced significantly in the past several years so that reversing a procedure once thought of as permanent is now highly possible.
Vasectomy reversal: Outpatient Procedure
Vasectomy reversal can generally be performed on an outpatient basis, allowing the patient the opportunity of returning to his home or a nearby hotel rather than having to stay in the hospital. This saves considerable expense and makes the overall experience much more pleasant.
Operating time for a vasectomy reversal typically ranges from 2½ to 3½ hours, depending on the complexity of the surgery. A general anesthetic is usually used. It is recommended that out-of-town patients stay in Denver one day following surgery prior to returning home. Post-operative care should include an office visit two or three weeks following surgery to evaluate the healing process and a semen analysis at six weeks. Monthly semen analyses are then obtained for approximately 4-6 months or until the analysis results stabilize.
Vasectomy Reversal Success
It should be remembered that much of the success of a vasectomy reversal depends on two factors: (1) the skill and experience of the surgeon and (2) the findings at the time of surgery. Regarding surgical skills, the individual who operates more frequently will certainly increase his technical expertise. State-of-the-art vasectomy reversal involves the use of microsurgical techniques to reconnect the vas deferens, allowing return of sperm to the semen. The use of a surgical microscope allows the surgeon to use suture material so tiny that it is difficult to see with the naked eye.
Return of Sperm and Pregnancy Success
As mentioned previously, one important factor in determining a successful outcome is the surgical findings. When the vas is opened, fluid will flow from the testicular side of the vasectomy site. If sperm are present, then we expect roughly 90% of patients to have return of sperm with an associated 60% to 70% pregnancy rate. If no sperm are present but the vasal fluid is clear and free-flowing, then the likelihood of a successful outcome decreases somewhat with the chances of subsequent pregnancy being about 40%. If sperm are not identified and the fluid that is found is thick and pasty, then a connection of the vas to the epididymis (the gland that collects the sperm from the testis) should be performed. This procedure yields a successful outcome in approximately 30% to 40% of cases. The procedure wherein the vas deferens is divided above and below the site of the previous vasectomy and then reconnected is termed a vasovasostomy. When the vas deferens must instead be connected to the epididymis, the procedure is referred to as an epididymovasostomy.
Vasovasostomy
There are a variety of techniques available for vasectomy reversal. In all cases, the surgeon’s goal is to obtain precise alignment of the ends of the vas deferens and achieve a watertight closure. Attention to these details will help prevent scarring and obstruction of the repair. The use of an operating microscope greatly facilitates the achievement of a satisfactory result.
The two most widely accepted techniques for vasectomy reversal are the so-called modified two-layer closure and strict two-layer closure.
Modified two layer closure
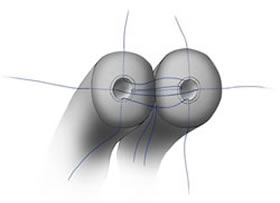 |
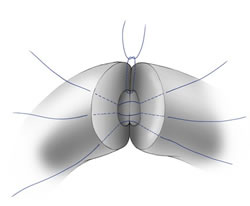 |
Figure 1: Vasovasostomy Modified Two-Layer Closure
In the first technique (shown in Figure 1), four to six microscopic sutures are placed through the full thickness of the vas deferens to align the inner aspect (lumen) of the two cut ends. A series of sutures are then placed in the outer layer of the two ends to prevent sperm leakage and potential scarring or breakdown.
Strict Two-Layer Closure
In the strict two-layer closure (figure 2), multiple sutures are placed in the inner aspect of each end which do not pass through the full thickness of the vas deferens.
 |
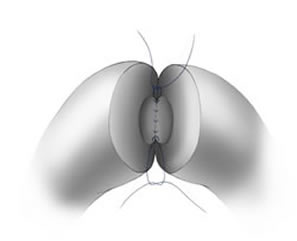 |
Figure 2: Vasovasostomy Strict Two-Layer Closure
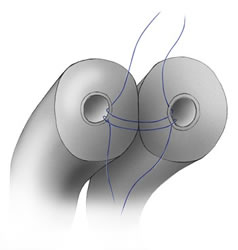
A separate layer of sutures are then used to close the outer surface as illustrated in Figure 3.
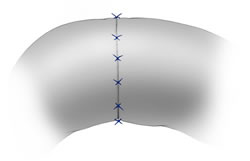 |
Figure 3 |
Results gathered from a large series of vasectomy reversals do not show a clear advantage of one technique versus the other. The choice of technique depends largely on the performance of the surgeon as well as the condition of the vas deferens at the time of surgery.
Epididymovasostomy
Experience has shown that if the vasal fluid contains no sperm and is thick and pasty, simple reconnection of the vas deferens will often meet with poor results. In this situation, the surgeon should be prepared to connect the vas directly to the epididymis (epididymovasostomy). In this procedure, the epididymis is explored and when sperm are identified, the cut end of the vas is sutured to the epididymis at that point using a microsurgical technique. Epididymovasostomy is a very technically demanding procedure and generally is only undertaken by experienced micro-surgeons.
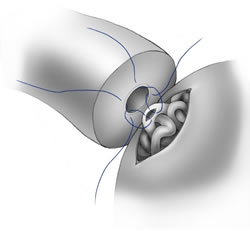 |
Figure 4 |
Regardless of the technique used for vasectomy reversal, careful attention to detail is vital to achieving a successful outcome. As more is learned about this procedure as well as the entire field of male reproduction, the prospect of reestablishing fertility following a vasectomy is constantly improving.
In performing a vasectomy reversal, a vertical incision is made on each side of the scrotum. Holding sutures are placed in the tissue surrounding the vas above and below the site of the previous vasectomy, and the vas is divided at those two points. The limb of the vas leading to the urethra is irrigated with saline to insure that it is not obstructed. Fluid from the limb of the vas leading from the testicle is then examined microscopically for the presence of sperm. As mentioned before, the presence of sperm in this fluid indicates an improved prognosis. The vas ends are then brought into position near each other with a holding suture and joined using the microsurgical suture technique described earlier.
For additional information on vasectomy reversals use the following links:
Read more about our vasectomy reversal specialist, Dr. Randall Meacham.